🧐#2: What Happened To You? by Oprah Winfrey and Dr Bruce Perry - Book Summary and Key Takeaways
What "counts" as trauma? | What do the long term effects of trauma look like? | What does being dysregulated mean? | Post Traumatic Wisdom and Healing
Welcome to the second edition of the newsletter! Thank you to each and every single one of you who have subscribed and are reading! ❤️🙏
This week’s book is the ultimate reframing of “What’s wrong with you?” into the much more useful, productive and empathetic, “What happened to you?”
It is ultra-readable, written as a conversation that goes back and forth between its authors Oprah Winfrey and Dr Bruce Perry. It has case studies, their own personal experiences, great questions and explains the science and research of trauma in a digestible format compared to many other science heavy texts.
Here are the key takeaways, questions and answers. An advance warning that there is a lot of information packed in here 🤯 because there is just so much incredible value in the book I wanted to share with you, so I’d encourage you to scroll through and read the questions and sections that resonate! Quotes in italics are taken directly from the book.
What is trauma? What “counts” as trauma?
This is something I have heard time and time again from people. They are unsure if what they have been through is “bad enough” to “count” as trauma. That if they haven’t been to war or kidnapped that they haven’t experienced trauma.
“For most people trauma means a really bad event or experience, usually one that “sticks,” that you don’t forget, and that can have an enduring impact on you.” - page 93
What this means is that you are the only person who can truly know or be the judge on your own trauma and what has impacted you, because it is just that - impact on you.
Trauma isn’t something that is judged by an external standard or by comparison to someone else, or checking what has happened to you against a shopping list of events published online.
Here’s a story from the book to illustrate:
“There’s fire at an elementary school. A veteran firefighter can walk right up to the flames and put them out, business as usual. In contrast, a first-grader witnessing his classroom burst into flames will experience minutes of intense fear, confusion, and helplessness.
This illustrates one of the key issues in understanding a potentially traumatic event: How does the individual experience the event? What is going on inside the person; is the stress response activated in extreme or prolonged ways? In other words, because the internal experience of a given event varies from person to person, so does the long-term impact.
Imagine that while the first-grader reacted to the fire in his classroom with terror, a fifth-grader in a different part of the building didn’t feel as threatened. To him, the fire was almost exciting; because he was further from the direct threat, he felt safe the entire time. So we have three people in the same event, each experiencing it differently. And because each experienced it differently, each had a different stress response. Based on her years of experience and practice, the firefighter had a moderate activation of her stress-response systems; the event felt predictable and controllable. For her, it was a resilience-building experience.So do we say the fire was a trauma? For the first-grader, yes, but not for the fifth-grader. The fifth-grader had an “acute stress reaction,” and within weeks returned to his baseline. And for the firefighter, as we said, it was a resilience-building experience.” - page 94-95
This is a more obvious and singular example of an occurrence of trauma. The other way that trauma can be experienced is through marginalisation or when there are repetitive, but less severe events:
Marginalized peoples—eg. through race, gender, sexual orientation, or anyone who is excluded, minimized, shamed—are traumatized peoples. To be excluded or dehumanized in an organization, community, or society you are part of results in prolonged, uncontrollable stress that is sensitizing. Marginalization is a fundamental trauma.” - page 212
Trauma is ultimately defined by the 3 E’s:
The Event: ie. The fire in the classroom
The Experience of the individual in that moment: ie. complete terror, couldn’t escape, risk of death (first-grader) vs a fairly usual part of their working day (fire fighter)
The Effects: these are explored in the next section
What do the long term effects of trauma look like?
The effects of trauma can impact someone in 4 different areas:
😖 Intrusive symptoms - These include recurring, unwanted images and thoughts of the traumatic event, and dreams or nightmares about it.
🙅♀️ Avoidant symptoms - where someone either knowingly or subconsciously avoids places, videos, things or people that remind them of the original traumatic event.
🥺 Changes in mood and thinking. This can include depressive symptoms—sadness, loss of pleasure from anything, a sense of guilt, an overfocus on negative things, and basically a feeling of emotional and physical exhaustion.
💥 An alteration in arousal and reactivity. These are symptoms related to the sensitized stress-response networks being overactive and overly reactive. They include anxiety, hypervigilance, increased startle response, high and variable heart rate, and sleep problems.
The most confusing thing about some of these effects—especially the categories of avoidant and alteration in arousal and reactivity—is that you might not realise that these things are even happening to you, or that you are reacting to something.
[If you want to know more about this, I’d recommend reading pages 107-112 in full.]
What does it mean to be dysregulated due to trauma?
“Regulation is also about being in balance. We have many different systems that are continuously monitoring our body and the outside world to make sure we’re safe and in balance.
Stress is what occurs when a demand or challenge takes us out of balance—away from our regulated “set points.”
When we get out of balance, we become dysregulated and feel discomfort or distress. When we get back into balance, we feel better. Relief of distress—getting back into balance—activates the reward networks in the brain.” - page 45
Our level of functioning depends on the state we are in - this is true for everyone, not just those who have been affected by trauma.
As we shift through different emotional states—outlined along the top row of the table—from Calm > Alert > Alarm > Fear > Terror, the amount and type of access we have to our cognitive abilities changes:
The key difference between those affected vs those not affected by trauma is this: People sensitised by trauma can escalate more quickly into those states of dysregulation, or be triggered to escalate by a lower threshold of stimulus.
In the next figure down, if you follow the blue line that is labelled “SENSITIZED” you will see how that person can end up in a state of Fear or Terror on a daily basis, triggered by their usual environment. Compare that to those “NEUROTYPICAL” and “RESILIENT” where it takes moderate and high levels of stress before they result in the upper emotional states.
(Side note: I loathe the use of the word Resilient as it implies that those who are sensitized are not also resilient, where the two groups have had vastly different opportunities and environments for development and/or healing.)
Why does it matter if we are regulated or dysregulated?
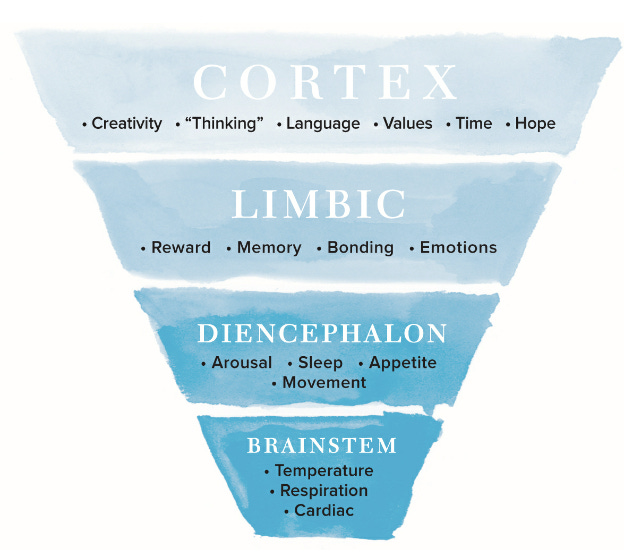
Simply, when we are dysregulated the part of our brain that we have control over goes offline and becomes inaccessible. To best understand this, we need to do a quick lesson on which parts of our brains are responsible for what functions.
There are 4 levels or departments of control in our brains:
🫀 The bottom level is the Brainstem. It controls temperature, breathing and keeps our heart beating. Basically, everything automatic that keeps us alive that we don’t have to think about.
😴 The next level up is the Diencephalon. It is in charge of our sleep, hunger, thirst and movement. So it’s those things that are also very basic to our staying alive, but that we need to make some decisions about meeting our needs like what to eat and when to go to sleep.
👨👨👧 The second top level is the Limbic System, which is getting more sophisticated. It influences bonding with other people and meeting our emotional needs.
👩🎤 Finally we get to the top with our Cortex. This is everything that makes us who we are as individuals. It controls our decision making, our planning, our creativity, our values, our problem solving, our language and the ability to tell time—that is to think in terms of the present, past and future.
The more dysregulated—ie. the more stressed, frightened, under threat or in danger—we become, the less we have access to the upper parts of our brains.
If you take a moment to scroll back up to Figure 6, the bottom row reflects functional IQ when in each emotional state, going from 100-120 in a Calm state and plummeting down to 60-80 when in a state of Terror.
Here’s an example of this at work:
Take one of Dr Perry’s patients, Mike Roseman. He was a war veteran who 30 years later was still having severe symptoms of PTSD. One night he heard a motorcycle backfire and all of a sudden he was lying on his stomach between two cars, covering his head. He didn’t remember but he also attacked his partner in the process, prompting them to raise this event in therapy.
Here is Dr Perry’s explanation to Mike of why and how that happened using the levels of the brain:
“When the cortex is ‘online’ and active, we can think about the past and look forward to the future. We know which things are in our past and which things are present. But there are no networks in the bottom part that think or tell time.
Input from all of our senses—vision, hearing, touch, smell—first comes into our brain in the lower areas. None of our sensory input goes directly to the cortex; everything first connects to lower parts of the brain.
Once the signal comes into the brainstem at the bottom of the triangle it is processed. Basically, the incoming signal is matched against previously stored experiences. In this case, the matching process connected the motorcycle backfire with gunfire—remember that combat-related memory?
And since your brainstem can’t tell time, or know that many years have passed, it activates the stress response and you have a full-blown threat response and become dysregulated. You feel and act as if you are under attack. Your brainstem can’t say, ‘Hey, don’t get so stirred up, Korea was thirty years ago. That sound was simply a motorcycle backfiring.’
Now, when the signal finally gets up to the cortex, the cortex can figure out what’s really going on. But one of the first things that happens when you activate the stress response is that systems in the higher parts of the brain, including our ability to ‘tell time,’ get shut down. So the information about the motorcycle backfire did ultimately get to the cortex, but it took a while. And until it did, you were back in Korea.” - page 21-24
How do we get regulated again once we realise we’re dysregulated? Or help someone else who’s dysregulated?
It is impossible to reason with a person who is dysregulated, whether that’s ourselves or others. They use the saying in the book:
“Regulate, relate, then reason.” - page 136
Getting regulated has to be the number one priority, because:
“If the person is regulated, you can connect with them in ways that will facilitate rational communication. But if they’re dysregulated, nothing you say will really get to their cortex, and nothing already in their cortex will be easy for them to access.”
This means to get regulated again and return to the Calm state, we need to rely on non-verbal, non-thinking strategies. By far the best way to do this is using rhythm.
Every person in the world can probably think of something rhythmic that makes them feel better: walking, swimming, music, dance, the sound of waves breaking on a beach. It’s why we rock babies when they cry.” - page 44
Colouring in (this is why those mindfulness colouring books are so popular!), focussing on your breathing, listening to music - any of these strategies can help someone get regulated again.
Each of us is different and will have our own individual preferences. If you are looking for ways to help yourself regulate, follow your gut and continue trying different things until you find something that works.
To close the loop on Mike Roseman from the previous example, part of his therapy to help him regulate was getting massages multiple times a week for a “bad back” (because it was easier to say it was for his back than for his mental health) and dancing to swing music and rock ‘n’ roll. This helped him keep himself in a state of Calm for longer periods, and return from dysregulation more effectively than he could before.
Post Traumatic Wisdom and Healing
Years ago, Dr Perry went to spend time with Māori elders to learn from their ancient healing practices. They told him that,
“The pillars of traditional healing are 1) connection to clan and the natural world; 2) regulating rhythm through dance, drumming, and song; 3) a set of beliefs, values, and stories that brought meaning to even senseless, random trauma; and 4) on occasion, natural hallucinogens or other plant-derived substances used to facilitate healing with the guidance of a healer or elder.” - page 193
He goes on to say that unfortunately our Western medical model fails to use all four of these methods well, focussing too heavily on psychopharmacology and therapy, greatly undervaluing the power of connectedness (1) and rhythm (2).
“A core element of all of the traditional healing practices was something the Māori called whanaungatanga. The word refers to reciprocal relationships, kinship, and a sense of family connection.” - page 241
Dr Perry laments the fact that Western methods fail to get to the heart of healing, to whanaungatanga.
“We heal best in community. Creating a network—a village, whatever you want to call it—gives you opportunities to revisit trauma in moderate, controllable doses.” - page 193
Connection is part of the cure.
In closing, if you or a loved one are struggling with the aftermath of trauma know that it is not because you are broken or that something is wrong with you, it is because something happened to you and your body and mind are responding in the best way they can in the circumstances.
Thank you for reading and I hope you gained something for your own personal toolkit or knowledge from this edition! I am here for you and am always a willing ear if you have any thoughts, questions or reflections bubbling up after reading.
Until next week,
❤️🙏 Eleanor
Additional links and resources:
If you are struggling, please reach out to a support service or professional:
🤝 Human Rights list of Mental Health Support Services
Dr Bruce Perry’s website has access to resources, a workbook that accompanies What Happened To You, as well as presentations, training and research publications:
🧠 Neurosequential.com
Next week’s book:
Coming out next Friday 11th Feb 2022 is the edition #3 of the newsletter, featuring:
📚 The Body Keeps The Score
by Bessel van der Kolk
If you haven’t already, subscribe to the newsletter here to receive it direct to your inbox!
📸 Follow Post Traumatic Growth Weekly on Instagram






Brilliant!!